https://www.freepressjournal.in/analysis/covid-19-march-will-soon-become-a-terrifying-sprint-in-india
Covid-19 — the government has been caught swimming naked
RN Bhaskar
Today is Tuberculosis (TB) Day. Unlike coronavirus, where a vaccine has yet to be developed – it could take anywhere between a year to several years – tuberculosis has a vaccine. It is called BCG. As the CDC points out (https://www.cdc.gov/tb/topic/basics/vaccines.htm), it is supposed to be given to infants and small children in other countries where TB is common. It is normally given only to children who have a negative TB test, who are continually exposed and cannot be separated from adults who have the TB strain. Unfortunately, BCG does not always protect people from getting TB. That could be the excuse government officials could take shelter under for not eradicating TB from India.
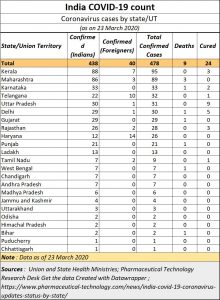 But when it comes to coronavirus, the government has been caught swimming naked. And the tide has run out. As of March 23, 2020, 438 people in India were affected by coronavirus, and 9 people had died (see table). But this may be a misleading number. The fact is that – in India – there is no clear estimate of numbers that have contracted coronavirus.
But when it comes to coronavirus, the government has been caught swimming naked. And the tide has run out. As of March 23, 2020, 438 people in India were affected by coronavirus, and 9 people had died (see table). But this may be a misleading number. The fact is that – in India – there is no clear estimate of numbers that have contracted coronavirus.
There was hardly any testing being done till now (even though the government finally decided to permit 12 private clinics to do the testing, five of which are in Mumbai). The government thus went against the basic recommendation of the World Health Organisation (WHO) – test, test, test. Without data from tests, one does not know the extent of the affliction, and what measures need to be taken.
Moreover, even while this article is being written, there is yet no clarity if the tests will be offered free of cost to patients, just as the government had initially insisted, or if they have to pay. The ICMR had stated that the cost for each test (either to the government or to the patient) would have to be under Rs4,500. Whether this is being observed is not yet known.
Yet, the inclusion of the 12 private clinics will at least allow more testing to be done, under conditions that are a lot more hygienic (https://www.indiatoday.in/india/story/coronavirus-in-india-12-private-labs-authorised-to-conduct-covid-19-tests-have-15-000-collection-centres-1658796-2020-03-23) . Each of these private clinics have several branches which can act as collection centres. People can be spared from the long queues, under unhygienic conditions, at the government-owned Kasturba Hospital in Mumbai till a few days ago — each person literally bumping into the person ahead. It appeared that the hospital too did not care for social distancing.
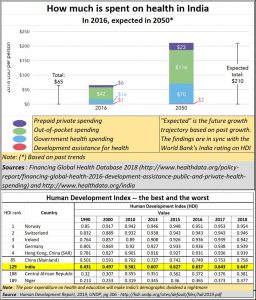 All this only helped highlight the abject unconcern successive governments have shown towards health services — and hence its people — till now. It spends barely 1.8% of its GDP on health services.
All this only helped highlight the abject unconcern successive governments have shown towards health services — and hence its people — till now. It spends barely 1.8% of its GDP on health services.
To understand how deplorable health services are in India, just look at the admission halls of the two largest government and municipal hospitals in Mumbai – JJ Hospital and KEM Hospital. The queues are long, the crowds are almost stifling. You don’t need a richer environment for viruses to spread. The irony is lost on the government which goes about shutting malls, cinema houses, even schools. It often forgets that the source of infection in India are usually the hospitals.
And do not forget the slums, abetted by politicians keen on creating vote banks. Common toilets – even for COVID-19 isolation wards — unwashed basins and a lot more (https://www.freepressjournal.in/mumbai/mumbai-patients-complain-of-poor-conditions-at-kasturba-hospital). More people in the slums are going back to open defecation because the common toilets are filthy, unusable. And now that we have coronavirus as an epidemic, how do you lockdown a slum? Do you starve its residents, or exterminate them by denying them their daily livelihood? Vexatious issues caused by terrible politician inspired gambits.
As the adjoining chart shows, India spends little on healthcare. Most people end up paying for medicare out of their own pockets. This is either because the public health services do not offer quality services, or they do not dispense treatment quickly enough. The result is that most people spend a significant part of their personal earnings on medicare.
That also explains why the World Bank ranks India rather poorly on the human development index (HDI). As the chart shows, India is barely above the levels of countries like Niger.
Yet, most government officials were sanguine till last week, pointing out that the spread of the infection had not gone too far. They forgot that COVID-19 is a deceptive virus. It appears to be benign, with symptoms like common flu. But it spreads rapidly. They refused to listen to the warmings of either China or the WHO. They thought they knew better.
It is only now that health administrators have gun to appreciate the gravity of the situation. They are being confronted with the mathematics behind the Covid-19 infection.
In this context, it is worthwhile listening to what Professor Jeremy Farrar has to say. He is a world expert on infectious tropical diseases. He was based in Vietnam for many years where he ran the Oxford University clinical research unit. He was responsible for research and response to the outbreaks of Swine flu, bird flu, SARS and Ebola. He is currently a director with Wellcome Trust. In a conference call with global investors on 25 February 2020, Professor Farrar made disclosed some very important findings (the full transcript of his talk can be downloaded from http://www.asiaconverge.com/wp-content/uploads/2020/03/2020-02-25_Wellcome-Trust-COVID19-25.02.pdf).
 He pointed out that the rate at which COVID-19 would spread depends on what is known as the “Arnot”. In the case of this epidemic, the Arnot is believed to be three, “… if I had the infection today, I would pass it on to approximately three other people. That doesn’t sound a very big number until you think that those three pass it onto three others and those people pass it on to three others.” Thus, one person being infected would pass it on to three which would become 9, then 27 and then 729 — all within hours or days. That is why containment plays such a crucial role in the spread of epidemics.
He pointed out that the rate at which COVID-19 would spread depends on what is known as the “Arnot”. In the case of this epidemic, the Arnot is believed to be three, “… if I had the infection today, I would pass it on to approximately three other people. That doesn’t sound a very big number until you think that those three pass it onto three others and those people pass it on to three others.” Thus, one person being infected would pass it on to three which would become 9, then 27 and then 729 — all within hours or days. That is why containment plays such a crucial role in the spread of epidemics.
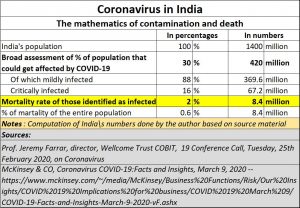
He goes on to add that “. . . in 2009 of the pandemics of H1N1 swine flu . . . 16% of the world’s population there were infected. And I think we can assume that that would be close to double that.” In other words, almost 30% of the world population could get affected. The percentages would be higher in countries where health services are primitive and lower where containment of the virus spread was excellently managed. According to him, “. . critical care . . . would be to about 12%. . . . . Case fatality in Wuhan is still around between two and 4%. . . . . . I would stick to about a 0.5 case fatality rate [for the world] . . . . . . I would still stick with an attack rate of a median of about 30% of the world’s population that would get infected with this on a range somewhere between 25 and 40.”
Now extrapolate these numbers with those for India. It has a population of 1.4 billion. You could now expect that at least 30% — if not more – of this population could get affected.
This could mean that around 8.4 million people could die if no steps were taken to isolate the contaminated and protect those who had not been infected. Of course, this also means that the number of deaths can be reduced, as has been the case in China, South Korea and Singapore. Or they could climb further – as in Italy and Spain.
The government appears to have woken up. It is aware that the WHO has already warned the world that the rate at which infections are spreading has been increasing. (https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—23-march-2020). As the WHO director general Dr. Tedros Adhanom Ghebreyesus stated on 23 March, “The pandemic is accelerating. It took 67 days from the first reported case to reach the first 100,000 cases, 11 days for the second 100,000 cases and just 4 days for the third 100,000 cases. You can see how the virus is accelerating.. . But we’re not prisoners to statistics. We’re not helpless bystanders. We can change the trajectory of this pandemic.”
The fact is that a surge in numbers could manifest itself in India soon. As Ramanan Laxminarayan, Affiliate Professor, Global Health, Princeton University, and Director and Senior Fellow, The Center for Disease Dynamics, Economics & Policy, points out, “India missed the bus on testing, and all that can be done now is to protect the elderly. . . . .It should lock down now, 3 weeks later it won’t work” (https://www.youtube.com/watch?v=2HvAWGuiyfE). He believes that India should ready itself for 300-500 million cases by July end without drastic interventions and possibly between 1 and 2 million fatalities. He calls for massive use of a simpler antibodies tests that he says private practitioners can easily execute. He also calls for private companies to manufacture ventilators on a war footing.
Reliance Industries, through HN Hospital, has already taken a lead in area. Besides setting up a dedicated 100 bedded centre at Seven Hills Hospital, Mumbai, in collaboration with the MCGM (Municipal Corporation for Greater Mumbai), it is also enhancing it production capacities to produce 100,000 face-masks per day and a large number of personal protective equipment (PPE), such as suits and garments, for the nation’s health-workers to equip them further to fight the coronavirus challenge. Expect more companies to follow suit, thanks to the vacuum generated by the government’s dismal services in this area
We are in uncharted territory partly because of the absence of data on account of little testing done). Thus we do not really know how the disease will spread. For now, the government has announced a lockdown in 75 coronavirus-hit districts across the country (https://www.freepressjournal.in/india/coronavirus-update-after-reporting-positive-cases-75-districts-in-india-to-go-under-lock-down). Trains have been shut down till 31 March, and so have schools. But the basic question remains – how do you lockdown thousands of slums (URL) which are largely politician abetted (http://www.freepressjournal.in/analysis/slums-show-disrespect-of-politicians-for-democracy-r-n-bhaskar/1358963)?
Then there are states which are veritable blackholes. For instance, one of India’s poorest (and most populated) states in Bihar. Little data is forthcoming from the state except that two cases tested positive, and one person died. The numbers are just not credible.
Says Dr. T Sundararaman, former director of the National Health Systems Resource Centre, in an interview with media (https://timesofindia.indiatimes.com/india/low-testing-could-explain-indias-small-covid-numbers/articleshow/74661955.cms), the low coronavirus rates in India could be on account of low testing. “Bihar has only one testing centre . . . . . Having just 52 centres across India makes no sense. And not even all of these are fully functional.” It must be clarified here, that these remarks were made before private players were allowed to get into the area of testing.
India had time and advantage on its side. It could see the way China and the WHO had coped with this virus. Both had been transparent about their strategies and recommendations. India should have been prepared for the crisis. Singapore and South Korea studied the numbers well. Countries like Italy, and now even India, did not. Now the price is being paid for in human lives.
What is amazing is the way Singapore has managed to keep its Covid-19 death rate to near zero despite doing what is not conventional logic. As of 23 March, it had 365 cases, of which 340 were hospitalised, 152 discharged, 15 critical, and just 2 deaths (https://www.moh.gov.sg/covid-19). It has not promoted the use of face masks, though it does insist on hygiene, especially washing of the hands. Schools are not closed, nor are offices. But health monitoring systems can be found in schools, in offices at stations and in other public places.
If a person is suspected of having contracted coronavirus, isolation measures immediately kick in. Treatment is free for both Singaporeans and foreigners, because the government knows that the cost of not treating the person could be a lot higher. Confirmed cases are promptly isolated. Medicare then gets limited only to people requiring it.
And when it comes to daily wage earners, the state even gives a small sum ($100 per day) to those people who have been deprived of their source of income. More details of about this amazing achievement, with zero death rates as of now, can be gleaned from the 10 minute address of Singapore’s prime minister Lee Hsien Long on 12 March 2020 (https://www.facebook.com/125845680811480/posts/3111854648877220/). Thus, in Singapore life goes on as normal. It knows business and commerce are equally important for the health of a nation as is protection from viruses.
The only ban that has been imposed is that on public gatherings, conferences, religious meetings and the like. India’s legislators love bans. That could explain why every two days, there is a list of “thou-shalt-nots”.
Till India’s testing and data collection are ramped up several fold, we may not even have the numbers of the dead or dying. Do bear in mind that India, with its population of 1.4 billion, could test barely 6,000 people each day nationwide. Compare this with the 8,000 people who are tested daily in the US, 9,000 in Japan, 12,000 in France, 13,000 in the UK 13,000), and 23,000 in Italy. South Korea has conducted over 200,000 tests till which is why, say experts, Korea has seen declining numbers (https://indianexpress.com/article/explained/india-coronavirus-tests-icmr-6317845/).
It is quite possible that the present epidemic will make India’s policymakers to sit up and create rules that discourage the formation of slums (http://www.asiaconverge.com/2020/02/aadhaar-cards-populations-many-ways-rig-numbers-financial-transactions/) and encourage the creation of more doctors and hospital beds (http://www.asiaconverge.com/2018/08/ayushman-bharat-great-concept-doctors-overlooked/). Currently, India has just 1.3 hospital beds and 0.8 physicians for every 1,000 people.
Can India undertake a course correction now? Hard to say. It is quite possible that the coming two weeks will compel India’s policy makers to do a major overhaul of its health services and the processes underlying them.


































COMMENTS